And there are many reasons you might want to do this, including the fact that the shorter your billing cycle, the more reliable your cash flow. The document printed with patient demographics updated includes a list of specific services to record diagnoses. When a patient contacts a healthcare provider, the details of the condition and the service provided are recorded, either in form of audio or video. These details might be documented in front of the patient or after the interaction. It clarifies the condition and prescriptions provided by the healthcare professional.
Would You like to Increase Your Collections?
- This stage creates a thorough patient profile, which paves the way for correct invoicing.
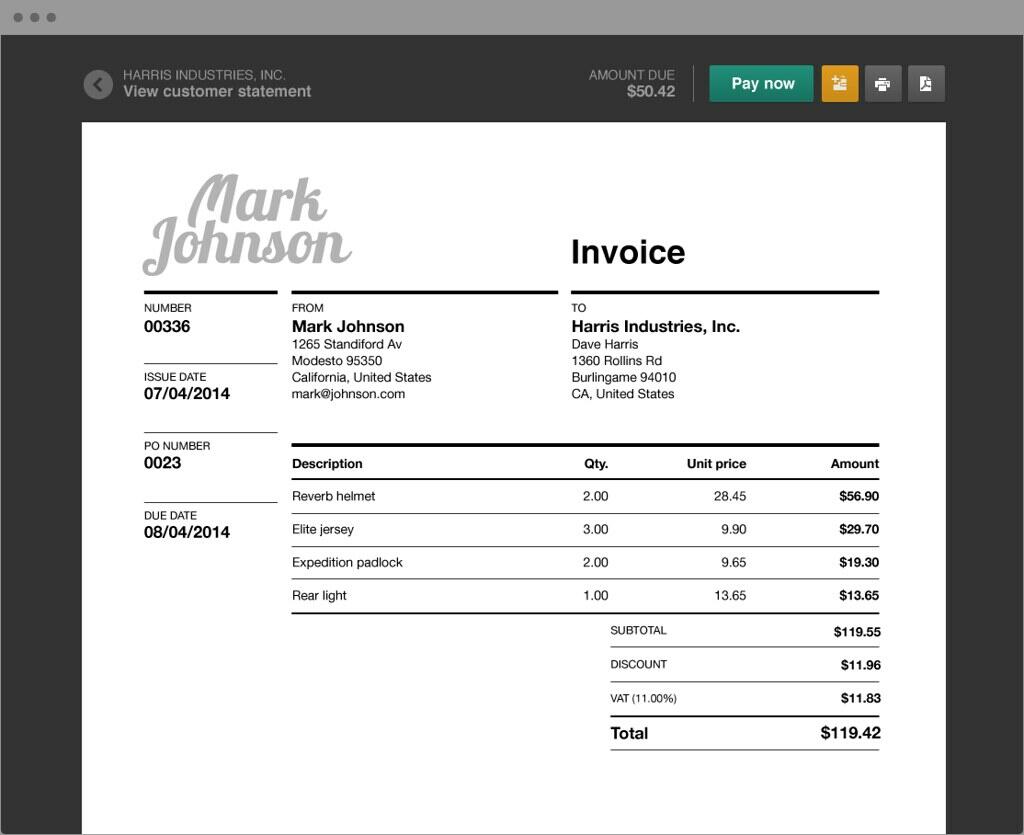
- Coders submit the codes and corresponding charges to the payers, and then providers bill patients for the remaining balance.
- If they cannot agree, they must go through an independent dispute resolution process to determine the payment rate.
- Managing the revenue cycle and monitoring KPIs can effectively prevent revenue loss.
- For example, an apartment complex may issue a bill for rent on the first day of every month, regardless of when tenants signed their individual leases.
The second step in the process is to determine financial responsibility for the visit. This means looking over the patient’s insurance details to find out which procedures and services to be rendered during the visit are covered. If there are procedures or services that will not be covered, the patient is made aware that they will be financially responsible for those costs. Medical billers submit claims directly to the payer or use a third-party organization, such as a clearinghouse.
Difference Between Direct Primary Care vs. Concierge Medicine
With rising claim denials, increasing regulatory complexity, and the need for advanced technology, optimizing RCM has never been more critical. GeBBS Healthcare Solutions offers comprehensive, technology-driven solutions to help healthcare providers, including FQHCs, streamline their RCM processes, reduce denial rates, and ensure compliance. With GeBBS as a partner, healthcare organizations can medical billing cycle steps focus more on patient care while providing a healthy revenue stream. In the healthcare system, medical billing is a complex procedure involving the organization and submission of claims to insurance companies or government health programs. By acting as a common language, the coding helps healthcare providers be paid and guarantees accuracy, compliance, and openness in financial dealings.
Point of service collections
Arduous administrative work, ever-changing regulatory guidelines, accessing and managing the correct data, and other hurdles can slow the process and result in lower rates of reimbursement. When the claim makes it past the https://www.bookstime.com/ clearinghouse to the payer, the data file is processed, converted to a claim form for the claims analyzer or claims adjudicator to review. The clearinghouse report should show when a claim has been received by the payer.
HOW COVID-19 IMPACTED MEDICAL BILLING AND CODING
Insurance coverage differs dramatically between companies, individuals, and plans, so the biller must check each patient’s coverage in order to assign the bill correctly. Certain insurance plans do not cover certain services or prescription medications. If the patient’s insurance does not cover the procedure or service to be rendered, the biller must make the patient aware that they will cover the entirety of the bill.
- One of the fundamental steps in obtaining a medical license to practice medicine and assist patients is credentialing.
- The medical office staff will make a copy of their Insurance Card to get their information in the system.
- The medical biller takes the superbill from the medical coder and puts it either into a paper claim form, or into the proper practice management or billing software.
- The notes from the physician are converted into a medical transcript, either by the in-house team, or a third party that specializes in medical transcription; voice recognition software is often used.
- Vindicating this information now will help help billing problems and detainment in the future.
It will benefit your billing and rendering staff and give your case a further comprehensive medical history for future reference. A medical coder must review this information after the meeting to apply the proper canons to the visit. Verify that you have the case’s insurance information up to date and accurate during enrolment. You should also find out if any fresh visits bear billing, depending on the nature of the appointment( worker’s compensation, accident, etc.). Using Medical Billing Software can help you make the insurance process easier. Medical billers and coders are fortunate to enjoy flexible work schedules since numerous enterprises allow them to work from home or in the office.

 TARJETAS GRÁFICAS
TARJETAS GRÁFICAS